GPs have voted to strike if some contract changes, including forcing practices to open on Saturdays, are not withdrawn. The doctor proposing the motion at the British Medical Association’s annual conference in Brighton urged her fellow medics to ‘channel our inner Mick Lynch‘. This analogy – and the meeting’s decision in favour of industrial action – tells us everything we need to know about the political leanings of the BMA who ought to be unbiased. It was particularly distasteful to invoke a comparison with the RMT’s rail strike which caused travel chaos and distress last week for NHS staff and their patients, among other innocent casualties.
The main quarrel of the meeting was the demand by NHS England that GPs should provide a full service on Saturdays from 1 October. Clearly the intention of these extended hours is to offer patients greater access to GPs. Difficulty in obtaining face-to-face appointments with a doctor has been the commonest complaint from patients, especially during the pandemic. But some doctors, it appears, don’t seem to care.
Industrial action by GPs to offset this demand is laden with hypocrisy given the working practices of most GPs. GPs currently have no contractual responsibility for patient care outside weekday office hours, nor for urgent care at night, over weekends or bank holidays. This concession was negotiated between the BMA and the Labour government in 2004 and has directly contributed to the exponential pressure on A&E. Almost six in ten GPs work three days per week or fewer: this is another reason why patients cannot always access general practice. Yet the Royal College of GPs rarely mentions these facts in its pronouncements.
Needless to say, some GPs do their best to provide the highest quality of patient care. But for many patients the efforts of a minority of doctors isn’t enough. Put simply, they need to be seen by a doctor. And if their GP surgery is shut at weekends, they are all too likely to turn up at hospital, putting further pressure on the NHS.
Even if Saturday working was adopted, it is likely that additional sessions would be done by locum GPs. The instruction by NHS England for GP practices to open on weekends was sure to have been music to the ears of the National Association of Sessional GPs (NASGP). Their website describes a membership of 6,000 doctors which is ‘growing fast’. NASGP offers a management structure to deal with bookings and billings and claims to have provided locum doctors to over 2,000 practices. Yet this pattern of work can make it hard to provide continuity of care, which is the service patients most value. The many advantages of regularly seeing the same GP – including familiarity with the patient’s history and medication and a greater chance of identifying red flag symptoms for earlier detection of cancer – risk being lost.
So what’s going wrong? Data published recently shows that between 2014 and 2021, the number of fully qualified GPs in the NHS dropped by seven per cent. Experienced GPs are leaving the NHS because of ‘burnout’ and for punitive pension reasons. Meanwhile, newly qualified UK graduates are reluctant to fill the gaps unless they have a reason to work part-time. Only about 8,000 British doctors graduate annually, and between 2016 and 2021, we recruited 53,296 doctors from abroad, many from low-income countries where they are needed to provide essential services. This practice raises moral and ethical questions. And given that we don’t know where these doctors end up working – and there is no evidence they are working in local surgeries – it is not clear that even this influx of doctors can address our GP problem.
It’s true that not all of the BMA’s resolutions were unreasonable, especially the demand for an increase in salary for junior hospital doctors, whose vital contribution to the NHS has long been unappreciated. In his address, Dr. Chaand Nagpaul, the retiring Chair of the BMA Council, correctly referred to the ‘plight’ of junior doctors, many of whom have graduated with a debt of almost £100,000. Today’s junior doctors are tomorrow’s consultants and their starting salary after six years in medical school is abysmal at £29,384. At less than half the annual salary of an experienced train driver, this remuneration is partly responsible for the tragic decision by about 20 per cent of UK-trained juniors either to abandon medicine or to practice outside the UK. That loss is unsustainable, given that, in 2021, 63 per cent of new doctors registering with the General Medical Council qualified abroad.
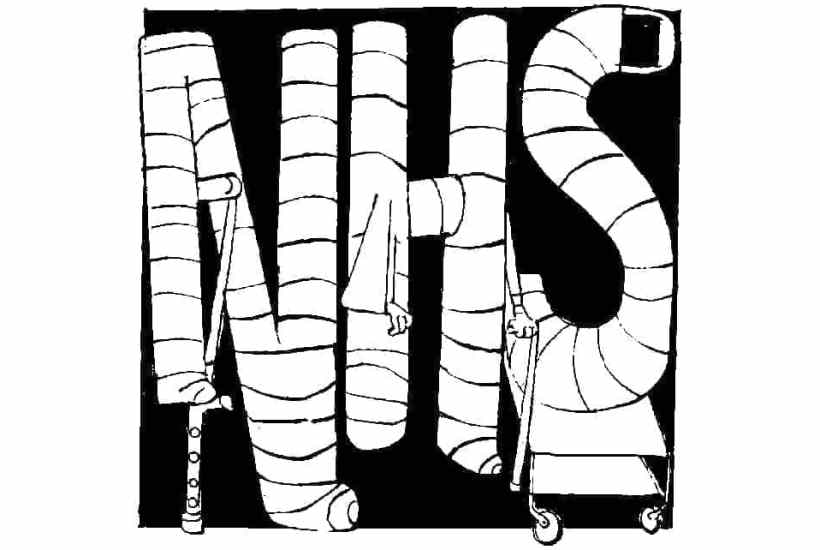
But while the BMA has a point about this, it’s reluctance to stomach a shake-up of working hours to better meet patients’ demands is hard to take. General practice is broken. Why didn’t delegates at the BMA’s Annual Representative meeting discuss methods for its resuscitation rather than details of their new contract?
Got something to add? Join the discussion and comment below.
Get 10 issues for just $10
Subscribe to The Spectator Australia today for the next 10 magazine issues, plus full online access, for just $10.


















Comments
Don't miss out
Join the conversation with other Spectator Australia readers. Subscribe to leave a comment.
SUBSCRIBEAlready a subscriber? Log in