Every generation has an event that defines it. For my father, it was the Second World War. For his father, the First World War. Some might have thought Brexit would have been ours, but the coronavirus pandemic puts politics into perspective. There is no doubt that 2020 will be viewed by historians in the same way 1918 is now: as the year of the plague. Tens of thousands have died and the death toll continues to rise sharply. The global economy is in tatters. The world is in lockdown. But if any good can come from coronavirus it might be in the way in which we come to think – and talk – about death. It’s been said that in Britain today we view death in the way Victorians did sex; as one of life’s great unmentionables. Might our current predicament change that?
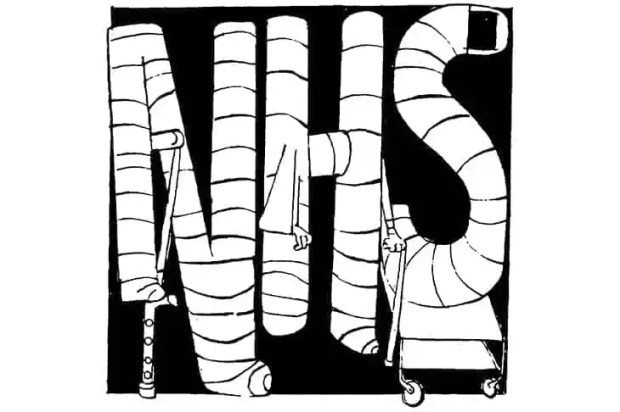
The pandemic has certainly changed some things for the better. When coronavirus first took hold in Britain, the speed with which the sometimes sclerotic and glacial apparatus of the NHS moved rapidly into preparing for the coming onslaught was something to behold. Departments of health boards and trusts that barely knew of each other began to cooperate. Organisations previously vying for the same resources became collaborators. The scale of the task ahead became clear in a meeting of consultant staff in my hospital just before lockdown started in March. A colleague explained how a model used in a briefing by Chris Whitty, the chief medical officer, predicted a hospital death toll of several hundred people a week in a health board of our size in the very worst case scenario. It was a daunting moment. Some of us had been in touch with colleagues in northern Italy and understood the kind of near-apocalypse that might quickly overwhelm the health service. We hoped for the best and prepared for the worst, knowing that even in a good scenario, the death toll would be high.
The actual scale of events proved more manageable than some feared. Yet the awful reality of the impact of this virus is still shocking. Leaving aside arguments about whether or not deaths have been preventable, the death of everyone who has died from or with Covid-19 is a life cut short and a tragedy for those who love them. More certain than the debate about the handling of coronavirus is the simple reality of the prolonged and difficult bereavements that will afflict the loved ones of those who have died in recent weeks. Husbands and wives and sons and daughters, restricted by travel limitations, social distancing or necessary but strict limits on who could keep the last vigil, never got a chance to say goodbye. Funerals have been small, muted affairs with most family and friends excluded.
The impact on those caring for coronavirus victims in hospitals should also not be overlooked. A cohort of junior doctors has had a crash course in the practical care of the dying and their loved ones in conditions that were far from ideal. Those staffing the frontline wards have seen large numbers of deaths in a very short period. This may be the tempering steel of a medical generation. It may be the cause of future professional and psychological trauma. Only time will tell.
My job, unlike most (with the exception, perhaps, of clergy, registrars and undertakers) brings me face to face with death, anticipated or actual, every day. A key task for health care staff like me over the past two months has been the rapid implementation of advance care planning. This involves being clear with patients and their families about plans for managing this illness. Should invasive ventilation be attempted? How far should doctors go down the road of aggressive medical intervention? If such interventions are made, might they work? Or could they simply prolong suffering? When is the right moment to accept that a person’s time might have come?
This pandemic is a grim wake up call for a generation that has not faced the types of conflict endured by our parents and grandparents. Yet it’s important to think about coronavirus, not as unprecedented, but conversely as something of a distraction. The nanometres-small collection of RNA and associated molecules which forms this virus is merely the latest expression or vector of death. The modes by which we die have changed over millennia of human history. For much of history, death has come through famine, violence or war. For many centuries until the last, death came through now largely treatable infectious diseases. In more recent decades, death comes in the slow trajectory of degenerative disease. Medicine changes the mode of death. It prevents it for a time, but can never defeat it finally.
It is important then that we use this opportunity to take stock of life and death. When the crisis is over and we are free to enjoy life again, we should savour every day. Yet the crisis should also give us some cause to examine how we approach death. To discuss with those we love, while we can, how we would wish to go. How far we would want physicians and surgeons to intervene when our bodies become old and frail and where the decent limits to medicine lie. What is proportionate in holding on to life at its end?
Sadly, this is unlikely to happen. When the flu pandemic of 1918 ended, it went largely forgotten for decades. Despite a death toll far outstripping that of the First World War, interest in the pandemic was overtaken by the Great Depression (to which, arguably, it was a significant contributor), the chaotic world politics of the 1920s and ‘30s and another World War. Academic interest in the pandemic only really took off in the early years of the 21st century following further outbreaks of influenza in the Middle- and Far East. It is likely that even in a world more connected than ever that our current troubles, when they are over, will be quickly forgotten. It may be that this latest brush with mortality might give us pause to think about how we die, as individuals and as a society. We should. But once the pubs open again, we probably won’t.
Paul Keeley is a consultant in palliative medicine at Glasgow Royal Infirmary <//>
Got something to add? Join the discussion and comment below.
Get 10 issues for just $10
Subscribe to The Spectator Australia today for the next 10 magazine issues, plus full online access, for just $10.


















Comments
Don't miss out
Join the conversation with other Spectator Australia readers. Subscribe to leave a comment.
SUBSCRIBEAlready a subscriber? Log in